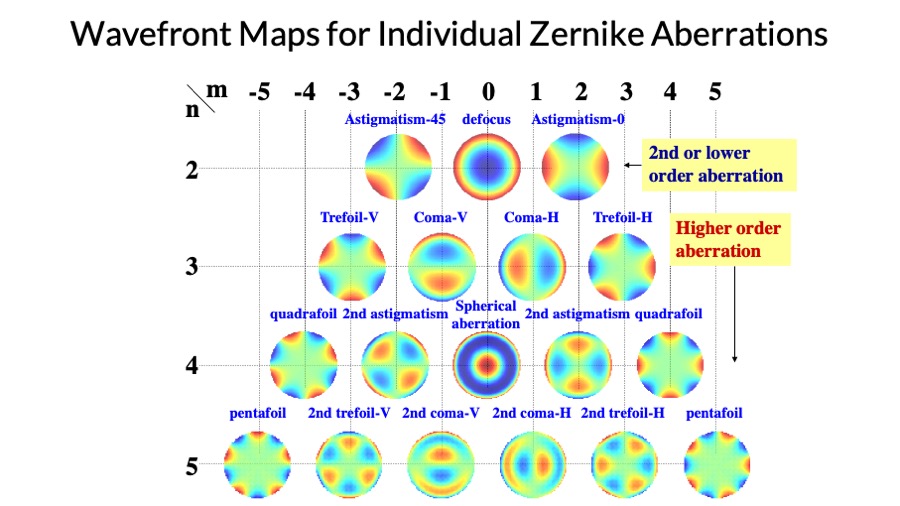
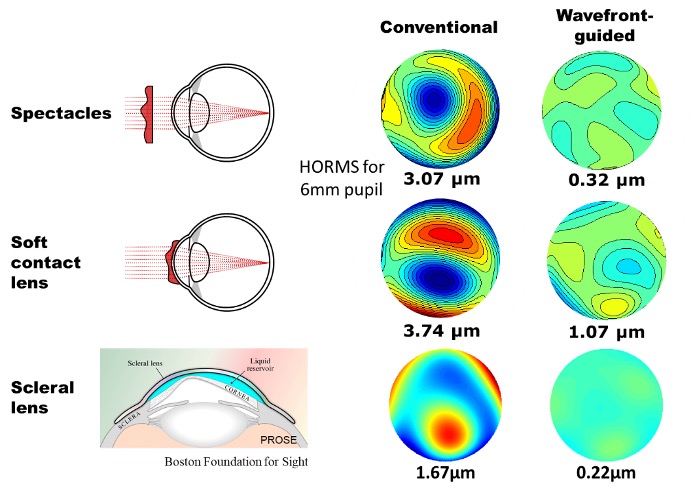
When improving vision by correcting the ocular aberrations, it is important to take the aberrations of the whole eye into account (as opposed to corneal aberration only) since retinal image quality is determined by the total aberration. quantifying aberrations of the cornea and internal optics as well as the whole eye found that corneal and internal optics aberrations can neutralize each other to certain degree.
This provides evidence that the whole eye aberration, when viewed as aggregated data, is actually smaller than the combined aberrations of the cornea and internal optics when considered (and measured) in isolation. This is clinically important because if an eye’s aberration correction is based, for example, on the corneal aberration measured with corneal topographer, the outcome will be sub-optimal.
It should be noted that with a conventional scleral lens, it is true that the majority of the corneal aberration is compensated due to the reduced refractive index difference between the cornea and tear/fluid lens created underneath the lens. However, the residual higher order aberration is still significantly larger (see the 3rd row in Figure 5) compared to measurements from typical normal eyes. Again, this is due to the various internal ocular components – i.e. the posterior corneal surface and the crystalline lens – in addition to the uncorrected aberrations from the anterior corneal surface.
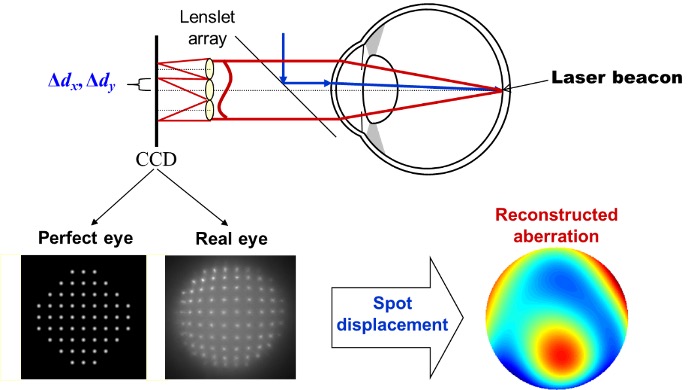
The other important factor to be managed carefully, in order to maximize correction performance, is the alignment of wavefront guided optics to the eye. This is because significant amounts of decenteration and/or rotational mis-orientation of the wavefront guided optics can make visual quality even worse, compared to conventional optics. It is therefore critical to identify the reference axis along which the correction is applied. More importantly, this reference axis varies significantly between different patients.
Until recently, such research and development on aberrometer and wavefront guided optics was done in scientific research labs. The aberrometer was built on an optical bench, and analysis and lens design were done somewhat manually. The resulting optical design meant contact lens manufacturers had to develop their own technological and engineering capabilities to transfer the data to their lathe machine in order to precisely manufacture the irregular surface. This entire process took considerable time and required significant resources from both research lab and lens manufacturer.
OVITZ believes this is the main reason why such technology has not been commercially available – until today.
We have dedicated our enthusiasm and resources to developing an all-in-one system consisting of a commercially affordable aberrometer, wavefront-guided lens design, and a streamlined lens manufacturing procedure. Considered together as an integrated, closed-loop system, they complete the entire measurement and manufacturing process in a totally automated fashion (Figure 6). The OVITZ xwave system addresses the aforementioned critical issues by measuring the whole eye aberrations and registering the correction axis – customized to the individual patient.